Clinical Rotations
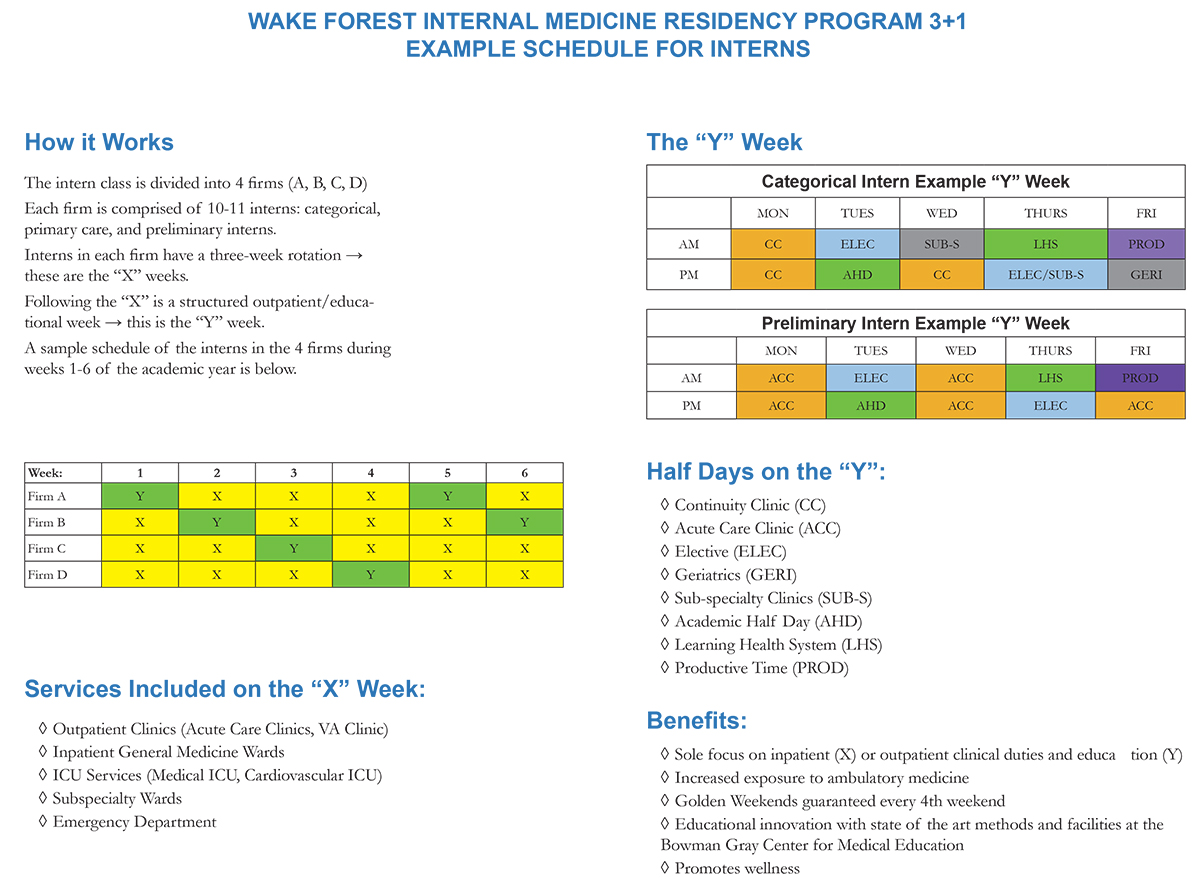
Intern Year (House Officer-1/HO-1)
The intern year offers broad exposure to direct patient care in internal medicine. Throughout the year, interns manage diverse patient populations and learn directly from subspecialists in a variety of inpatient services and outpatient clinics.
Our 3+1 model showcases three weeks on an “X” service (wards, ICU, nights, urgent care clinics, VA clinic, emergency department) followed by one week on a "Y" service (ambulatory medicine). The intern year is structured as an X+Y schedule, with 13 three-week rotations. The three-week X-rotations include the following dedicated experiences:
- 10 blocks of inpatient wards (including general medicine and subspecialty wards, night medicine, Cardiovascular Intensive Care Unit [CVICU] and Medical Intensive Care Unit [MICU])
- 1 emergency medicine block (ED)
- 2 ambulatory blocks, including the VA (categorical and primary care interns) and Acute Care Clinic
General inpatient medicine rotations are completed at both Atrium Health Wake Forest Baptist Medical Center, a traditional Level 1 Trauma Center and tertiary care hospital in Winston-Salem, as well as at Atrium Health High Point Medical Center, offering experience in both a traditional academic and community hospital setting.
The remaining ambulatory training will occur on the 13 “Y-weeks.” The Y-week features a variety of clinic experiences and educational conferences.
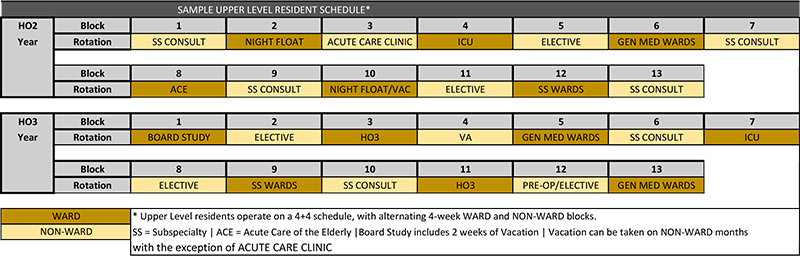
Upper-level Years (House Officer-2 and -3/HO-2 and -3)
The second and third years of residency are designed to facilitate your growth and maturation into a skilled internist. Upper-level residents manage the general medicine and subspecialty inpatient services (cardiology, hematology/oncology, leukemia, nephrology and geriatrics). Additional blocks include night float coverage and the MICU and CVICU.
Remaining blocks include:
- Subspecialty consults and clinic experiences
- Private practice internal medicine clinic
- General medicine acute care clinic and VA outpatient clinic
- Elective time tailored to the resident’s interests
- Inpatient procedures service
Elective time allows upper-level residents to tailor their schedule to their interests. Most residents schedule at least one research block.
During the HO-2 and HO-3 years, the schedule follows a general structure of alternating between four-week ward services and four-week non-ward rotations. Each of these years consists of 13 four-week blocks in this 4+4 format. Continuity clinics take place during the non-ward rotations only and are not scheduled during inpatient ward services. Resident continuity clinics are organized into practices and residents have two half-days of continuity clinic per week during their non-ward blocks that include dedicated sessions for ambulatory quality improvement. Coupling this 4+4 schedule with the 3+1 structure in the intern year allows for improved overall team continuity and full dedication to inpatient training for both upper levels and interns on ward services.
Example Upper-Level Resident Schedule
The content of the upper-level years is as follows: