About
The COMPASS Study is a cluster-randomized, pragmatic trial to implement and evaluate comprehensive transitional care versus usual care on patient-centered outcomes after stroke or transient ischemic attack (TIA).

Background
- Half of stroke and TIA patients are discharged home into a post-acute care system that is fragmented.
- These stroke and TIA survivors have multiple co-morbidities, poor risk factor knowledge and management, residual disability, and high readmissions.
- Effective transitional care, is an increasing priority in US healthcare, may optimize functional recovery and secondary prevention.
- Centers for Medicare and Medicaid Services (CMS) has established priorities and reimbursement for transitional care programs like COMPASS.
Design

- Forty acute care hospitals in North Carolina were randomized to either the COMPASS intervention or Usual Care.
- Over 6,000 patients discharged home were recruited.
- The primary outcome was functional status (SIS-16) 3 months after discharge.

Intervention
- A patient-centered intervention uniting transitional care and elements of early supported discharge
- The comprehensive care model intervention was consistent with CMS
- The intervention included a 2-day follow-up phone call, a clinic visit to comprehensively assess the patient include patient preferences and social determinates of health for an individualized patient care plan and referrals to rehab and community resources.
Results
Primary Conclusions
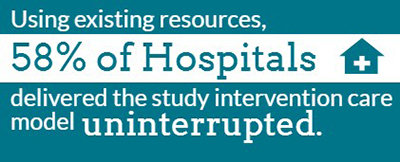
- COMPASS transitional care was not easily incorporated into systems of care.
- Only 35% of patients received the intervention. This was due to hospital delivery of care interruptions and to patient non-adherence to follow-up care.
- Functional status was similar by treatment group in intention-to-treat analysis.
Secondary Considerations
- Within intervention hospitals, patients who received the intervention had clinically meaningful improvements in key outcomes such as functional status, satisfaction with care, mortality, falls, disability, and depression compared with patients who did not.
Conclusions
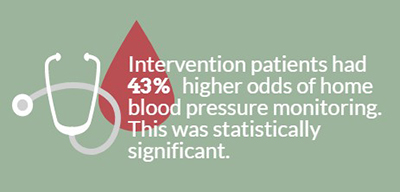 Intervention patients had 43% higher odds of home blood pressure monitoring relative to UC. Transitional care programs like COMPASS are a priority for CMS.
Intervention patients had 43% higher odds of home blood pressure monitoring relative to UC. Transitional care programs like COMPASS are a priority for CMS.- The pragmatic nature of this trial provides a realistic measure of challenges with transitional care uptake and its impact as delivered in diverse, real-world practices
- Implementation research is needed to identify strategies for optimal uptake of transitional care.
- When received, COMPASS may provide meaningful benefits to patients.
- Post-acute transitional care should be the next frontier for quality improvement for stroke systems of care.
Funding from the Patient-Centered Outcomes Research Institute (PCORI) Award (PCS-1403-14532). All statements are solely those of the presenters and do not necessarily represent the views of PCORI or its Board of Governors or Methodology Committee.
