Our three-year curriculum combines busy clinical services with purpose-designed rotation experiences to give you the experience you need to practice excellent pulmonary and critical care medicine. Our fellows enjoy a great balance of direct and indirect supervision, with increasing autonomy as their skills grow. Specific workshops and lectures increase your medical knowledge and procedural competence in a safe learning environment. There are excellent opportunities for research, including fourth-year opportunities for those wishing to pursue a physician-scientist career.

Most of our clinical training is offered at the Atrium Health Wake Forest Baptist Medical Center campus, which operates 1,004 acute care, rehabilitation and psychiatric care beds. Within the main hospital are general medicine nursing units, 33 intermediate care and 85 medical-surgical intensive care beds. Learn more about Atrium Health Wake Forest Baptist. Fellows care for patients in three inpatient venues:
- Medical intensive care unit
- Surgical intensive care units (ICU)
- Pulmonary medicine inpatient consultation service
These are busy rotations, with the section averaging more than 800 inpatient consults and nearly 3,500 admissions to the medical intensive care unit (MICU) every year. During each rotation fellows are paired 1:1 with attending faculty for the rotation. During their first year, fellows are exposed to the entire spectrum of pulmonary and critical care diseases by spending time both in the ICU and on busy consultative services.
Inpatient Pulmonary Training
 Our inpatient consultation service averages more than 800 inpatient consults annually. Fellows partner with our inpatient COPD pathway, including our respiratory care navigators and nurse practitioner to create a seamless transition from hospital to office care. In addition, our fellows provide expert consultation for patients on all hospital services, including (but not limited to) general medical, general surgical, obstetrics and gynecology, transplant, oncology, burn surgery, cardiovascular surgery, and otolaryngology.
Our inpatient consultation service averages more than 800 inpatient consults annually. Fellows partner with our inpatient COPD pathway, including our respiratory care navigators and nurse practitioner to create a seamless transition from hospital to office care. In addition, our fellows provide expert consultation for patients on all hospital services, including (but not limited to) general medical, general surgical, obstetrics and gynecology, transplant, oncology, burn surgery, cardiovascular surgery, and otolaryngology.
Outpatient Pulmonary Training
Approximately 7,000 outpatients are seen in the pulmonary clinic annually. All fellows experience a longitudinal continuity care clinic where they care for patients with the full spectrum of pulmonary diseases as their primary pulmonary specialty physician. These clinics occur one day every week except when the fellow is rotating on an inpatient service. Additionally, all fellows rotate several times on our outpatient pulmonary medicine (OPPM) rotation. During this rotation, fellows do not have inpatient duties and they rotate through faculty general pulmonary clinics and subspecialty clinics in:
- Severe asthma
- Pulmonary hypertension
- Cystic fibrosis and bronchiectasis
- Lung nodule evaluation
Bronchoscopy and Pleural Procedure Training
 Fellows are part of our pulmonary procedure team (PPT), a team of pulmonologists with expertise in advanced diagnostic bronchoscopy, pleural procedures, and interventional pulmonology. Our section performs roughly 1,000 bronchoscopies (fiberoptic and rigid) per year. Fellows will develop competence in all aspects of bronchoscopy, including:
Fellows are part of our pulmonary procedure team (PPT), a team of pulmonologists with expertise in advanced diagnostic bronchoscopy, pleural procedures, and interventional pulmonology. Our section performs roughly 1,000 bronchoscopies (fiberoptic and rigid) per year. Fellows will develop competence in all aspects of bronchoscopy, including:
- Diagnostic bronchoscopy and bronchoalveolar lavage
- Fluoroscopic-guided bronchoscopy
- Endobronchial and transbronchial lung biopsy
- Transbronchial needle aspiration (conventional and ultrasound guided—linear and radial EBUS)
- Robotic shape-sensing bronchoscopy
Fellows will also acquire competence in pleural procedures such as:
- Pleural ultrasonography
- Thoracentesis
- Thoracotomy tube insertion and removal (tunneled and non-tunneled techniques)

Pulmonary Function Testing and Interpretation
Pulmonary diagnostic testing experience includes time learning clinical pulmonary physiology by interpreting pulmonary function tests, cardiopulmonary exercise tests, inhalation challenge studies and sleep studies.

Our Medical Center has several intensive care units. Our fellows gain experience in medical, oncology-specific, and non-medical specialty ICUs. During MICU rotations, fellows are the primary proceduralist and will develop expertise in invasive hemodynamic monitoring procedures, endotracheal intubation and mechanical ventilation, and ultrasound-guided intravascular access. They will acquire both the technical proficiency necessary for these procedures and judgmental skills essential to their appropriate use. Fellows take a graduated active role in leading patient clinical management with a clinical team including interns, residents, pharmacists, nurses, respiratory therapists, physical therapists, nurse case managers and an attending physician. They also play an active role as a medical educator to house staff from internal medicine, family medicine, emergency medicine, and anesthesiology. Second- and third-year trainees rotate in our oncology specialty ICU where they gain experience leading a team that includes advance practice providers (NPs and PAs). All our ICUs utilize bedside ultrasound and support a point-of-care ultrasound curriculum facilitated by our critical care faculty.
As a quaternary referral center, our ICU patient population has high acuity, including a high percentage of patients receiving vasoactive medications and mechanical ventilation. Fellows gain access to real-time data about our ICU population, and report daily in our quality and safety huddle to assist with our ongoing safety and quality improvement efforts.
Each fellow’s non-medical ICU rotations occur in specialty intensive care units, such as:
- Trauma and Emergency General Surgery ICU
- Burn ICU
- Neurocritical ICU
- Cardiothoracic ICU
Fellows participate in several conferences and workshops to build their clinical and research skills. Fellow academic half-day occurs every other Tuesday, and additional conferences are held midday throughout the week. Workshops are scheduled throughout the year, usually on a Tuesday as well. Examples of workshops include Airway Management, ECMO, Mechanical Ventilation, Basic Bronchoscopy, Advanced Diagnostic Bronchoscopy, Pleural Disease Management, Introduction to Research, and Research Design Skills. A typical weekly schedule is shown below.
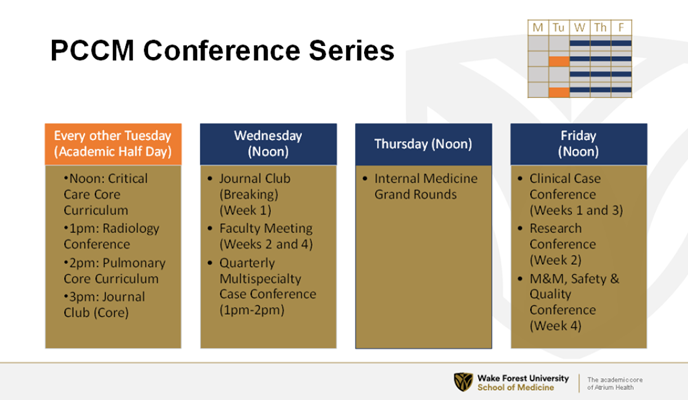
PCCM Conference Series
Every other Tuesday (Academic Half Day)
Noon: Critical Care Core Curriculum
l pm: Radiology Conference
2pm: Pulmonary Core Curriculum
3pm: Journal Club (Core)
Wednesday (Noon)
Journal Club (Breaking) (Week 1)
Faculty Meeting (Weeks 2 and 4)
Quarterly Multi specialty Case Conference (1pm-2pm)
Thursday (Noon)
Internal Medicine Grand Rounds
Friday (Noon)
Clinical Case Conference (Weeks 1 and 3)
Research Conference (Week 2)
M&M, Safety and Quality Conference (Week 4)
Outpatient Pulmonary Clinic
Dr. William Mariencheck, Jr.
A very important part of the pulmonary practice, and I would say an extension of the hospital-based critical care and consultative services, is the ability to provide care to the patient outside of the hospital in our continuity clinic. We're fortunate to have a beautiful facility that's located five minutes from the main medical campus.
Dr. Karl Thomas
And the patient experience is a little bit different than coming to the main medical center. We wanted a place where the patients could easily get to, with open parking and no elevators, and a straightforward way just to walk into the clinic.
Dr. William Mariencheck, Jr.
The outpatient practice, again, I think is fundamental to who we are as lung doctors. There's a great deal to be learned by following these patients over months and years, and our fellows are fortunate to have, as part of their training, a very robust continuity clinic where they have their own panel of patients. They will meet new patients in the office, referred in for the whole variety of general pulmonary needs, they will also inherit some of the graduating fellows' patients to continue to follow, and they can also follow up patients that they meet either in the ICU or on the consult service.
Dr. Karl Thomas
In that location, people might be surprised to learn that we have a sleep lab, they might be surprised to learn that we also have full pulmonary function testing, and they might be surprised to learn that we have an allergy group right there and we provide allergy immunotherapy shots right there in that same location.
Kaitlyn Grubb
So for our allergy clinic, we offer a wide variety of things for our patients. We can do food testing, environmental testing. We have venom and insect testing ability for our patients that have anaphylactic reactions or even just allergic seasonal allergy-type issues. The sleep clinic, we see a lot of narcolepsy patients, and we also see a lot of sleep apnea patients. We are thankful to have a sleep lab right there in the clinic so we can show the patients where they're going to be sleeping and what to expect. We offer daytime studies for our narcolepsy patients, and we offer nighttime studies for our sleep apnea patients.
Dr. Karl Thomas
That makes it a really very unique pulmonary, sleep medicine, allergy immunology environment. There's very few places across the country that would have all of that in the same location.
Kaitlyn Grubb
We have a great group of people that work in the Charlois Clinic every day, and I get compliments from our patients how really from start to finish how great their care was. Lots happening behind the scenes. I think a lot of that goes back to our triage nurses, and they are working very closely with the pulmonary physicians and the pulmonary fellows. Also, our biologic nurses are all working together to make sure that the patients are cared for in a timely manner and that they're taken care of.
Dr. Karl Thomas
The fellows in the clinic will see a wide range of patients with pulmonary disorders or sleep disorders, and if they want, allergy disorders, but the expectation is that they return to that clinic on a regular basis to see the same patients because then there's going to be a wide range that they'll see, including interstitial lung disease, pulmonary hypertension, asthma, COPD, as well as some other more esoteric diseases, including sarcoid, for example. So there should be a wide range of clinical experiences that they can have, not only with the diseases, but also with the patients and the patient's journey.
Kaitlyn Grubb
Our fellows have a really big role in our clinic. They have two full day clinics. They have their own schedules, and they, of course, have a attending there to supervise them.
Dr. William Mariencheck, Jr.
So we have a graduated volume of patient encounters in our fellow continuity clinic, starting with a lower number of patient encounters per half day and building each year up to a bit higher number. I think if you asked our fellows, I think that they're quite satisfied that their volume is not overwhelming, and in fact, as they approach second and third year, they're often asking, "How do we get more patients into our clinic?"
Dr. Karl Thomas
In my own clinic, a lot of their experience will be an experience of shared decision-making with the patients as they work through their problem, usually around cancer and cancer-related biopsies.
Dr. William Mariencheck, Jr.
From an administrative end, there are opportunities, as well. We have, like all pulmonary providers across the country, a need for better patient access. Fellows who have an interest in either clinical or organizational operations of an outpatient practice, we have great opportunity in that regard to help make things better.
Kaitlyn Grubb
They really get to develop taking care of their patients because they see them in clinic, some of them saw them in the MICU, and then they really follow them when they're at home. When calls come in, it goes back to the fellow, so they really learn how to not just care for a patient acutely but chronically over a long time.
Research Training
 The faculty and fellows in our section are engaged in several areas of research. During the first year of fellowship we hold an Introduction to Research rotation that provides new fellows with a view of available research activities and mentors. Each fellow identifies a primary project and mentor, and during the second and third fellowship years has ample protected time to pursue this project.
The faculty and fellows in our section are engaged in several areas of research. During the first year of fellowship we hold an Introduction to Research rotation that provides new fellows with a view of available research activities and mentors. Each fellow identifies a primary project and mentor, and during the second and third fellowship years has ample protected time to pursue this project.
Each fellow class participates in research workshops plus their scheduled research rotations. For fellows interested in establishing a research career, support is offered to apply for a fourth year of training. Learn more about research opportunities for our fellows.
All senior fellows present a section conference where they summarize their work. Each year many of our fellows also present their work for national audiences at conferences such as ATS, CHEST, and SCCM. Fellow projects frequently result in peer-reviewed publications.
