What if living independently longer was as simple as keeping your blood pressure down?
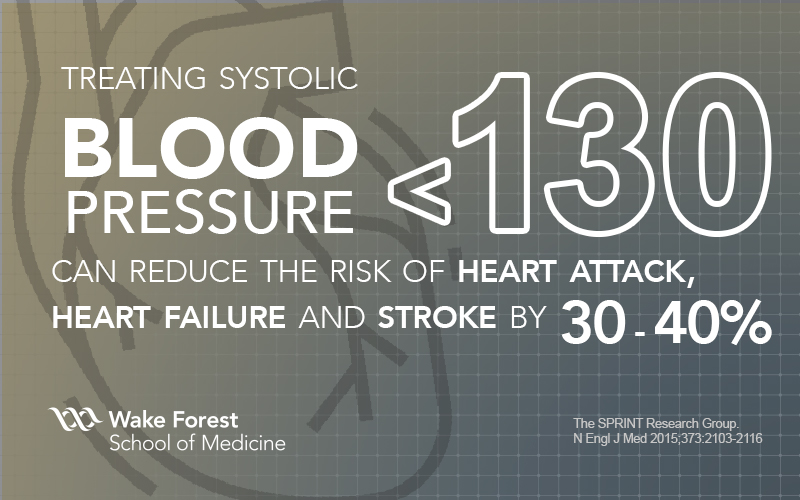
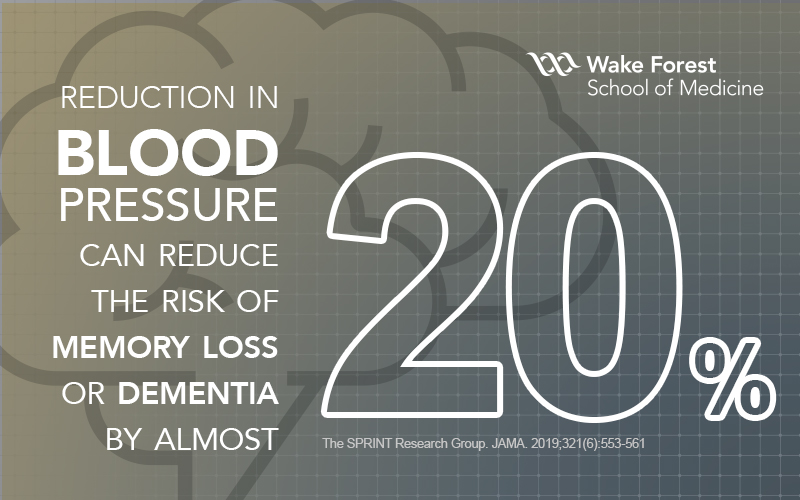
Wake Forest School of Medicine was a key contributor in the findings that demonstrated lowering blood pressure to below 130 mm HG (the top number in a blood pressure reading) in people, especially older people, can reduce the risk of heart attack, heart failure, stroke and death by 30-40%.1 Expanding on these findings, our researchers published more in 2019 from the SPRINT MIND study, showing that such a reduction in blood pressure can also reduce the risk of memory loss (early dementia) or combined early or late dementia by almost 20%2—the first intervention in history that clearly showed efficacy in reducing the risk for memory loss.
“We all knew lower blood pressure control had a significant impact on long-term health but it had never been scientifically validated,” explains Jeff Williamson, MD, director of the Center for Healthcare Innovation (CHI) at Wake Forest School of Medicine, section chief of Gerontology at Wake Forest Baptist Health and a lead scientist on the publication.
But this is only the beginning of the story.
CHI IGLOO
“When we have a major discovery, it can take 15 to 20 years to get it into the actual care environment,” says Williamson. He is referencing what is often called the “translational gap” in the medical community—the harsh reality that most scientific organizations don’t have the infrastructure to quickly move new knowledge gained into practice and that the individuals who usually identify the medical solution aren’t the ones who ultimately bring it to patient care.
 With 30 years of gerontology research under his belt, Williamson became restless with this inefficiency in health care, which in part led to the creation of the Center for Healthcare Innovation (CHI)—a unique group that sits between the School of Medicine and Wake Forest Baptist Health, acting as the “air traffic controllers” of scientists, digital experts, project managers and others that are working together to accelerate discovery into practice. “We don’t want osmosis to be the process by which discovery is implemented,” he says. “We want to be intentional and make it happen much more rapidly—thus the Center for Healthcare Innovation.”
With 30 years of gerontology research under his belt, Williamson became restless with this inefficiency in health care, which in part led to the creation of the Center for Healthcare Innovation (CHI)—a unique group that sits between the School of Medicine and Wake Forest Baptist Health, acting as the “air traffic controllers” of scientists, digital experts, project managers and others that are working together to accelerate discovery into practice. “We don’t want osmosis to be the process by which discovery is implemented,” he says. “We want to be intentional and make it happen much more rapidly—thus the Center for Healthcare Innovation.”
One of CHI’s major projects, the IGLOO Project (Implementation of Guidelines for Lowering Blood Pressure), is focused on the blood pressure findings from the SPRINT study. IGLOO will speed up the traditional timeline and close the “gap” for implementing these new recommendations.
A New Approach
The Systolic Blood Pressure Intervention Trial, or SPRINT, was a federally funded trial that started in 2010 and involved almost 10,000 people age 50 or older across the United States and Puerto Rico. The findings were clear that treating to the lower target of less than 130 mm Hg reduced cardiovascular events and helped save lives in people from all walks of life, and a diverse racial, ethnic and cultural background.
Wake Forest was a key player in SPRINT, serving as the National Coordinating Center. The study generated an entirely new set of guidelines for controlling blood pressure, formulated jointly by the American Heart Association and the American College of Cardiology.

A more accurate measure will result in more accurate treatment so that patients are not over- or undermedicated.
That accurate measurement is crucial, but has always been seldom achieved. The importance of the metric goes beyond individual patients and their well-being—methods and their outcomes affect entire populations.
Elisabeth Stambaugh, MD, chief medical officer of the Wake Forest Health Network, says “Blood pressure is so important because it reflects the overall health of our population. As a leader, a big part of my role is to look at how we take care of all of the patients, looking at the whole group and finding our gaps. One of the best ways we can improve our blood pressure management for our whole population of patients is to get better at taking blood pressure.”
Enter IGLOO
But knowing or understanding that change is needed is not the same as seeing it put to work in clinics to improve patients’ health, prevent cardiac events and ultimately extend or save their lives.
“Blood pressure is sometimes overlooked because it is such a routine part of every clinic visit,” says Stambaugh.
That’s where IGLOO comes in. It is being pursued by Wake Forest’s CHI as part of its mission to accelerate translation of scientific and medical discovery from the academic world to clinical medicine. According to Williamson, “IGLOO was designed to more rapidly get these new findings into the patient care environment. I’m not aware of any other health system in the United States is actually doing a project like this.”
By creating infrastructure within the institution specifically designed to address the translational gap, Wake Forest believes it can not only bring innovation to patients faster, but also generate tested and replicable models that systems anywhere could integrate.
IGLOO is currently rolling out the updated blood pressure measurement protocol in Wake Forest Baptist’s network clinics, a group of 125 clinics and 450 providers, led by Stambaugh. “The IGLOO project is the first part of fully implementing the recommendations that came out of the SPRINT trial,” says Stambaugh.
LaShanda Brown, PhD, MSN, is CHI’s research nurse manager. She works directly with clinical professionals to implement IGLOO. The protocol calls for blood pressure to be measured twice in patients with an automated cuff, with the average of the two readings taken as the final result. She says that the procedure is based on what she calls “practicing the pause.”
“They want you to wait five minutes before you check a blood pressure so that you’re not rushing a patient in to do a quick blood pressure assessment when they may be winded or tired or distracted or excited about their visit,” says Brown. As part of the roll-out effort, IGLOO encourages the clinics to educate their patients, particularly about why it’s important they take more time for this process.
“Patient education is going to be really important,” says Brown. “We’re working to introduce a streamlined process across multiple clinics.”
Primary care physician Yuri Cabeza, MD, was one of the first clinicians whose practice got involved with IGLOO. He is enthusiastic about the project and its benefits. “I tell my patients, ‘Look, when we talk about stats and we talk about blood pressure, I am trying to prevent you from having a stroke or a heart attack—cardiovascular death.’ We have the knowledge, so let’s try to do it!”
Data Rules
Part of IGLOO is the ongoing collection of data from the health care visits of each patient, which helps to measure and validate implementation success. A feedback loop is established.
As patient-linked data from the clinics accumulates in the electronic health record, the IGLOO model will be refined based on the lessons learned in the real world. As Scott Lang, IGLOO’s program manager at CHI, notes, “These guidelines are not one-size-fits-all. Pathways to better blood pressure control vary by incorporating weight loss, diet, exercise, and, often, medication. Everyone has a blood pressure, and it’s important to achieve the goal of < 130, but also based on the clinic, different patient populations have different needs. Our team has been good about telling the clinics, ‘This isn’t a top-down, you-have-to-do-it-this-way situation’—it’s a useful tool and were asking providers to use it as they see a need that is best for their patients.’”
The flexibility built into the implementation provides more robust data that contributes to refining the model. “What we’re learning is that when you do something like better blood pressure control in the pristine, ivory tower, ‘petri dish’ world of a clinical trial, you still need answers from out there in the real world. When you get out there, you realize that things like staff turnover and other factors are additional areas of scientific investigation,” notes Williamson. “That feedback loop is telling us, ‘OK, we need to come up with some better ways together to make sure that what starts well continues well.’ And that’s what a learning health system does.”
IGLOO is the embodiment of an important growing trend in medicine and health care called learning health systems—organizations or networks that continuously self-study and adapt using data and analytics to generate knowledge, engage stakeholders and implement behavior change to transform practice.
“The beauty of monitoring the clinic’s progress is that it takes you out of that individual focus of, ‘This is my patient and this is their outcome,’ to ‘How is the clinic doing as a whole?’ or ‘How am I doing over the course of a month?’” says Brown. “It shifts the individual working in isolation to ‘We have a team goal and we are going to work to this goal.’”
As the new method rolls out among the clinics, new data is being gathered that is helping adoption and implementation. The goal is to implement this new protocol in all of Wake Forest Baptist’s patient-facing clinics and services, not just the network clinics, and eventually across all of the Southeast through its partner organization, Atrium Health.
“One of the benefits of Atrium and Wake Forest coming together is that more people from diverse communities will be able to rapidly experience the benefit of research discovery in their lives through clinical practices,” says Williamson.
Stambaugh is excited about the vision to take the research that started in her clinics to the next level. “This is an amazing opportunity to be on the forefront of truly providing better care in blood pressure management and having a positive effect on a large population of patients,” she says. “If we can learn as we implement and try to refine the process, then we can spread that process that we’ve proven as a better way to do things across the Wake Forest Baptist Health family, across the larger Atrium Health enterprise family and then further across the entire country—and really show some amazing turnarounds in terms of blood pressure control.”
Bottom Line: Enhanced Health 
“The simple act of refining the procedure for accurately measuring blood pressure, along with the advances in management it fosters, promises vast rewards in enhanced health and longevity,” Stambaugh remarks.
IGLOO and the overall effort at Wake Forest to narrow the translational gap is designed to provide those rewards. “In my mind it is a win-win-win,” explains Williamson.
“It’s a win for our patients, because we can dramatically reduce their risk of having the disabling complications of heart failure, heart attack and stroke that often change their life forever. It's a win for me as a physician because I want to provide that best care. And it's actually a win for the health care system, because those very events; heart failure, stroke, heart attack, even death and dementia; they’re the things that are the most expensive forms of health care. If we can reduce that, we can free up money to be more innovative as a health care system and a society,” says Williamson.
“That’s a win for society, a win for us as practitioners, and especially a win for the patients and their families.”
The Center for Healthcare Innovation exists to improve care models and care delivery by applying research insights today and by bringing together the talent from both the academic, clinical sides, and in some cases, industry to make tangible change in patient care. IGLOO is only the beginning, but has proven that health care professionals are ready to eliminate the gap and proactively improve health.
1 JAMA. 2016;315(24):2673-2682. doi:10.1001/jama.2016.7050
Published online May 19, 2016.
2 JAMA. 2019;321(6):553-561. doi:10.1001/jama.2018.21442
Published online January 28, 2019.
3 JAMA Intern Med. 2019;179(3):351-362. doi:10.1001/jamainternmed.2018.6551
Published online February 4, 2019.
