Kate Callahan, MD, MS, associate professor of gerontology and geriatric medicine, is a geriatrician and a health systems scientist. Like many geriatricians, she cites the importance of one particularly important older person in her life.
By the time she was five years old, all of her grandparents had passed away. She ended up having a wonderful relationship with her childhood piano teacher, who became like an adopted grandfather to her. Later in his life, he developed a series of health problems, including delirium and weakness following a series of hospital stays. Callahan says he fell apart due to how he was managed in the health care system. “He became weak, tired, and confused, and I saw this incredible man who had survived the Nazis struggle to recover from the challenges of the health care system,” she says.
Callahan has devoted her career to improving conditions for older people, particularly those who are judged to be frail and are thus vulnerable to worse outcomes. She and her biostatistician research partner Nicholas Pajewski, PhD, associate professor for biostatistics and data science, are advancing a tool called the electronic Frailty Index (eFI). Together they run the eFI-cacious Lab at the Wake Forest School of Medicine and Wake Forest Baptist Health, a “laboratory” devoted to research and development of the eFI in order to promote patient-centered care of older adults.

“The health system is where we develop and test new approaches, and if they are effective or 'efficacious,' we implement them into practice for older adults.”
Kate Callahan, MD, MS
Overall, they are conducting research in health systems science. “The health system is where we develop and test new approaches, and if they are effective or “efficacious,” so to speak, we work to implement them into practice for older adults,” says Callahan. She calls it the science of change, which goes beyond the science of clinical medicine. With a time lag of 17 years for scientific innovations to enter practice and with less than 10% of new science ever being adopted, it is important to shift behavior in order to implement a different way of doing things to achieve a different outcome. That is the philosophy of the Center for Healthcare Innovation at Wake Forest, where there is a focus on older adults and their healthcare needs.
What is the eFI?
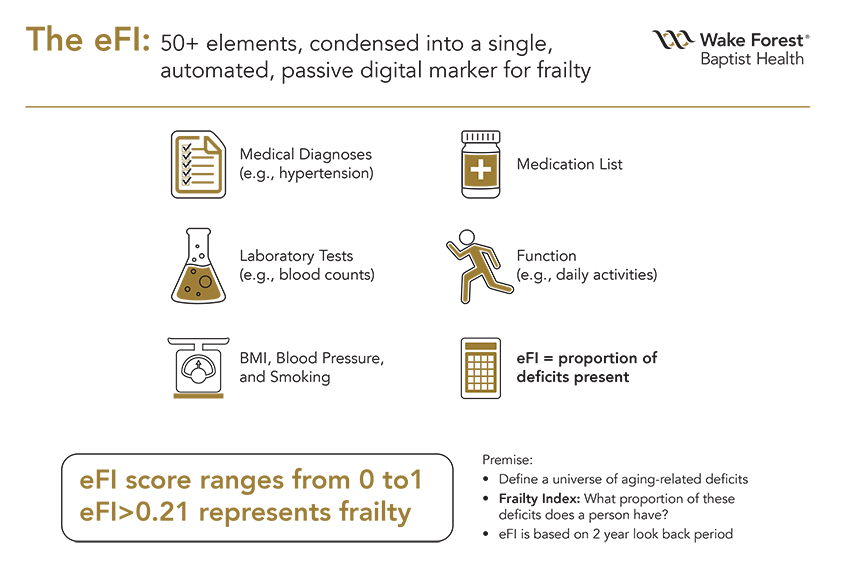
The eFI, as adapted by Callahan and Pajewski from work in Canada and England, is a tool embedded in the electronic health record designed to provide a comprehensive assessment of an older person’s frailty, or vulnerability to poor outcomes. Callahan expands on the concept of frailty:
“Understanding who is frail and who is not is critical to understanding the entire field of geriatric medicine, because age alone cannot help you make this distinction. When guiding an older adult through a medical decision, you want to know in whom there is adequate reserve that can carry people through challenging times, and in whom there is inadequate reserve. This is basically the definition of frailty: that someone has lost homeostasis. They don’t have the functional reserve or the physiological reserve that would help them bounce back from an infection or a trauma, and so if such a crisis comes along, they’re not going to handle it well. So some people will need additional services to help them go through an experience like a hospitalization or surgery. Our lab seeks to identify older adults with frailty and then test care pathways related to specific health quandaries, such as elective surgery or selecting a medication regimen.”
 According to Callahan, the challenge with frailty is that people think they know it when they see it. But the “eyeball test” is often not accurate or reliable. One study showed that 40% of elderly patients were re-classified after objective data was obtained. “Our eFI mobilizes data that are already present in the electronic medical record, and provides an additional set of information that makes our tool better at predicting outcomes,” she says.
According to Callahan, the challenge with frailty is that people think they know it when they see it. But the “eyeball test” is often not accurate or reliable. One study showed that 40% of elderly patients were re-classified after objective data was obtained. “Our eFI mobilizes data that are already present in the electronic medical record, and provides an additional set of information that makes our tool better at predicting outcomes,” she says.
The initial frailty index concept came from a Canadian team, who designed a lengthy list of questions to ask older people intended to measure their accumulated aging-related deficits. This frailty index showed the effectiveness of a simple ratio: that people with more things wrong with them would tend to have worse outcomes. A group in the United Kingdom subsequently determined how to use diagnostic data in the electronic health record to produce a frailty index—the first electronic version of the index.
The Wake Forest group takes the eFI a step farther. Unlike the British version, which is based solely on diagnostic codes, the Wake Forest eFI also includes blood tests, vital signs, and measures of physical and cognitive function, among other values. “You might have a situation where someone has a couple of high blood pressure readings, but they haven’t been formally diagnosed with hypertension,” explains Pajewski. “Our implementation would say there may be something going on with their blood pressure control without having that formal diagnosis.”
“The problem is that a lot of what I care about as a geriatrician isn’t in the charts; it’s not recorded on a regular basis,” says Callahan. So she and Pajewski started working on the expanded eFI in 2017, and received major funding for the project in 2018.
Pajewski says the Wake eFI is a more holistic approach than is often found. “It’s a view towards the whole person versus subdividing people into their diagnoses, which is how medicine typically works. You go to a cardiologist for your heart problem, you go to an endrocrinologist to manage your diabetes, etc. The geriatricians and primary care physicians are often much more focused on the integrative whole. I think the frailty index fits in that space.”
 “This eFI predicts healthcare use and healthcare outcomes, including such factors as overall health encounters, emergency department visits, hospitalizations and injurious falls,” says Callahan. The group found that on average frail folks had 8 times as many hospitalizations and 6 times as many falls. “We also found that the frail are more likely to die—a higher frailty index suggests higher mortality.”
“This eFI predicts healthcare use and healthcare outcomes, including such factors as overall health encounters, emergency department visits, hospitalizations and injurious falls,” says Callahan. The group found that on average frail folks had 8 times as many hospitalizations and 6 times as many falls. “We also found that the frail are more likely to die—a higher frailty index suggests higher mortality.”
The Electronic Geriatrician Will See You Now
The predictive power of the eFI contributes to helping determine when intervention is appropriate, and what form of intervention is called for. “People can live with frailty for some time, and we don’t get to opt out of taking care of people just because they are vulnerable,” Callahan explains. “You need to figure out how to intervene, but intervene in a way that is likely to preserve what matters most to older adults. Typically, if you ask them, they want to maintain as much of their independence as they can, and remain cognitively intact and as physically independent as possible.”
The eFI can help make those types of determinations in the absence of a geriatrician. “The method allows us to develop and test models that can provide effective population health management for frail older adults so that it is easier for frontline clinicians to care for folks who are frail,” says Callahan.

That expertise is critical in a time when geriatricians are in exceedingly short supply. There is currently a national shortage of geriatricians, and with the aging American population, the demand for geriatricians is projected to increase sharply in the coming years, while the supply is expected to increase only modestly.
"My dream is that eFI will be like a geriatrician at your fingertips.”
Kate Callahan, MD, MS
So a tool like the eFI could provide a crucial, essential service to caring for our elderly. “My dream is that we can think about the eFI to be like a geriatrician at your fingertips,” says Callahan. “It can help us identify folks who are likely to be more frail and then focus our energies on those individuals. The hope is that everybody can get geriatrics-informed care even if they’re not seen by a geriatrician.”
Beyond Geriatrics
The eFI-cacious Lab team envisions tremendous potential for applications of the index in many areas of healthcare. “There’s a vast opportunity,” says Pajewski. “The utility of the eFI is that it creates a tool that can be deployed across a health system, and that it would allow the language of frailty to be prevalent across all of those operations.”
"The utility of the eFI is that it creates a tool that can be deployed across a health system, and that it would allow the language of frailty to be prevalent across all of those operations.”
Nicholas Pajewski, PhD
The eFI is already being creatively deployed in several healthcare settings.
It is being used by the Wake Forest Surgical Navigation Center to assess frailty as a perioperative factor in deciding what an older adult may need to undergo surgery. “It can offer an instant assessment that’s predictive and scalable,” says Callahan. A study of the application has shown that a patient’s level of frailty can be an important element of length of hospital stay, discharge status, likelihood of readmission, or all-cause mortality. At 180 days post-surgery, “almost 10% of people who are frail will have died compared to about 2.5% of older adults who were fit,” Callahan states.
She notes that surgeons and anesthesiologists have their own “eyeball test,” a short assessment of how a patient is doing, called the ASA Physical Status Classification System, developed decades ago by the American Society of Anesthesiologists. Research has shown that the eFI increases discrimination beyond the ASA test to help assess patients pre-surgery. Also, surgeons used the eFI as a reverse filter for prioritizing elective surgeries in the context of COVID-19. “If the surgery is not critical and a person is perhaps frail, maybe we can wait a little bit and schedule the operation later,” Pajewski says, citing it as an example of how the eFI is already being used in the clinic.
 It is also being studied as a tool for clinical decision-making regarding Type 2 diabetes. Recent research has shown that aggressive glucose control may actually be counter-productive in frail older adults, and the eFI could help delineate who may benefit from a less-strict glucose regimen. “Older adults who have diabetes can get into real trouble with low sugars, and we may actually see higher mortality in people who are older and frail and have low sugars,” says Callahan. “We are at the early stage of evaluating whether the eFI can really change clinical decision making and improve outcomes in Type 2 diabetes,” adds Pajewski.
It is also being studied as a tool for clinical decision-making regarding Type 2 diabetes. Recent research has shown that aggressive glucose control may actually be counter-productive in frail older adults, and the eFI could help delineate who may benefit from a less-strict glucose regimen. “Older adults who have diabetes can get into real trouble with low sugars, and we may actually see higher mortality in people who are older and frail and have low sugars,” says Callahan. “We are at the early stage of evaluating whether the eFI can really change clinical decision making and improve outcomes in Type 2 diabetes,” adds Pajewski.
The eFI-cacious Lab team is continuing to develop new, innovative applications of the eFI. A case in point is the incorporation of data from Medicare annual wellness visits (AWVs). Among the goals of the AWVs are screening for cognitive function, physical ability, and memory issues. “It gives you a better glimpse into how the person is doing above and beyond their clinical diagnosis,” says Pajewski. “What the eFI does for the people who get these visits is to pull in that information and incorporate it into the overall assessment.” He notes that one of the questions in the AWV asks the patient to rate their own health on a one-to-five scale—how well they think they’re doing. “It turns out that that is a surprisingly good prognostic marker. If someone says they’re doing really badly, they’re probably going to do really badly.” He says that the prior measures have not incorporated that type of information. It’s one more example of the versatility offered by the eFI.
Enter COVID-19
In the wake of the COVID-19 pandemic, eFI research has understandably slowed, but the tool is also finding new applications as a result of the situation.
“People who are frail have, by definition, a lot of things wrong with them,” says Callahan. And faced with the threat of COVID-19, many patients are afraid of coming to the clinic. “We were approached by a Wake Forest Medicine population health staff member who asked, ‘Do you think we could use the eFI to target telehealth and find out what’s going on with our frail folks and just make sure they’re not getting lost in the shuffle during this?’” Nurse care managers reached out to almost 700 frail patients and thanks to the eFI found that more than 200 of them needed a clinic visit.
The eFI is an example of an important growing trend in medicine and health care called academic learning health systems.
When COVID-19 vaccines were first being distributed, they were in short supply nationally. So the eFI was used to prioritize among the 65-and-older population to ensure that the most frail people were getting vaccinated first. “Frailty is a major risk factor for death associated with COVID-19,” says Callahan. “So people using the eFI have been really smart and savvy about how they’ve been using it as a proactive implementation, such as the work with COVID-19 vaccine prioritization.”
Watch This Space
The eFI-cacious Lab team has ambitious plans for future applications of the technology. For example, Pajewski says he is working on developing machine learning and natural language processing techniques to access what he calls a “buried gold mine” of information hidden in clinicians’ notes about visits with patients. “We want to improve the eFI by bringing in what’s in the notes,” he observes. “Some groups have shown that especially when it comes to geriatric problems like dementia, falls, and issues with syncope and dizziness, that information tends to be in the clinician’s notes and not necessarily coded in the electronic health record.”
Pajewski also says the team is developing a technical embellishment to the eFI that will make it more portable and available to other groups beyond Wake Forest. “Right now the tool is tailored to the Wake Forest electronic health record system, so we want to make it more useful to other institutions without a great deal of effort,” he says. Eventually, the eFI may be marketed as a commercial product available in the healthcare marketplace.
Learning and Growing
The eFI is an example of an important growing trend in medicine and health care called academic learning health systems—organizations or networks that continuously self-study and adapt using data and analytics to generate knowledge, engage stakeholders and implement behavior change to transform practice.
Callahan, Pajewski, the many other members of the eFI team and their collaborators are poised to implement the many advantages offered by the tool and expand its capabilities. Ultimately, the eFI will allow our frail older adults the opportunity to live longer, safer, healthier, and more fulfilling lives by coordinating and refining care.
