Benjamin Franklin once said that “nothing is certain except death and taxes”; however, flu season might make the runner-up list. Every year, it rolls around, and we cross our fingers that the vaccine protects against the dominant strains of the influenza virus. Scheduling that shot is an annual event for millions of people.
But not everyone can receive a flu vaccine, and it’s not equally effective in all age groups. Newborns younger than 6 months cannot receive the vaccine, and after a lifetime of exposure to, well, everything, older adults’ immune systems may not generate a strong enough response. So how can we improve protection for those age groups?
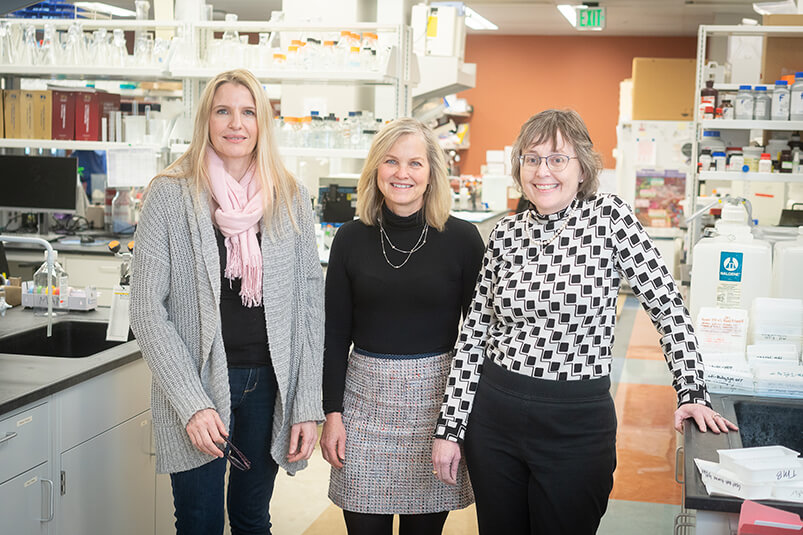
The Center for Vaccines at the Extremes of Aging at Wake Forest University School of Medicine is working on finding those answers. Martha Alexander-Miller, PhD, is a professor and the Dolores G. Evans, PhD Chair of the Department of Microbiology and Immunology at the school and director of the center, which was her brainchild. The leadership team for the center includes Karen Haas, PhD, associate professor of microbiology and immunology and of cancer biology, and Katherine Poehling, MD, MPH, professor of pediatrics and of epidemiology and prevention.
“There are significant challenges at both ends of the aging spectrum with regard to how good of a response you will make to a vaccine,” says Alexander-Miller. “At both ends, changes in the immune system affect the way that it functions and responds.
“What is altered in a newborn baby's immune system and what is altered in an older adult’s immune system are not the same things, but it results in the same outcome. The goal of the center is to understand how we might overcome the challenges associated with how the immune system functions in either the very young or the very old.”
The center aims to improve the safety and efficacy of vaccines specifically in those age groups, with an overarching goal of promoting all types of vaccine-related research as well as community outreach and community engagement regarding vaccines. Center members include basic scientists, clinicians and public health scientists, and their work benefits more than just the very young and very old.
“We have a whole host of other people who are less immune competent – for example, they have cancer or other medical conditions that cause them not to be as responsive,” says Alexander-Miller. “So, it is always my hope that what we learn from these two age groups can be transferred to help some of these other populations as well.”
 |
“What is altered in a newborn baby's immune system and what is altered in an older adult’s immune system are not the same things, but it results in the same outcome. The goal of the center is to understand how we might overcome the challenges associated with how the immune system functions in either the very young or the very old.” - Martha Alexander-Miller, PhD, Director of the Center for Vaccines at the Extremes of Aging |
Adding that extra ingredient
Adjuvants are one example of this. An adjuvant is simply a substance added to a vaccine that makes it more potent and encourages immune cells to respond. Alexander-Miller said that quite a bit of vaccine research focuses on both how to most effectively use the relatively few approved ones and the development of new adjuvants that may be more effective than current ones. And that’s a complex question to answer. Does a particular adjuvant work best in a particular vaccine? For a particular age group? If you add more than one adjuvant or an adjuvant that targets different receptors, will that improve vaccine response even more?
Alexander-Miller says the answers, at this point, are not clear. But she does think research will find that some adjuvant and vaccine combinations will work best for specific age groups.
Baby steps
Alexander-Miller’s research focuses on influenza vaccines and newborns and aligns closely with the center. But creating a vaccine that is safe for infants and effective has some unique challenges. For one, newborns’ immune systems are set up to deliberately not mount a large response to foreign substances. This prevents babies’ immune systems – to which everything is new – from going overboard and creating a dangerous amount of inflammation. This dampening mechanism is thought to be in place to allow microbiomes to become established throughout the body.
This means researchers have to find the very thin line of what is enough to overcome the natural dampening of infants’ immune systems so they generate antibodies while ensuring that the vaccines we give to our youngest people are as safe as they can be. Because when an infant – or anyone, for that matter – becomes infected with the influenza virus, it’s a race to see if the pathogen replicates or the immune system responds more quickly. Since babies’ immune systems are naturally somewhat muted, it’s more difficult to clear the virus, giving it more time to do damage or spread. This makes development of an effective vaccine for this group imperative.
Alexander-Miller hasn’t always studied developing effective vaccines in infants. But she reached a point in her career when she could make a shift, and helping the youngest, most vulnerable population appealed to her. Also, the proximity and availability of the Wake Forest University School of Medicine Vervet Research Colony, an NIH-supported national biomedical nonhuman primate research resource, provided access to a superlative model for study. Using the most cautious study design and approach meant someone was onsite in the nursery with the newborn primates 24 hours a day, 7 days a week, and every effort was made to maintain the highest levels of care. The results, Alexander-Miller says, were a rousing success and the newborn primates thrived.
More recently, Alexander-Miller received funding from Collaborative Influenza Vaccine Innovation Centers (CIVICs), a network of research centers funded by the National Institute of Allergy and Infectious Diseases, to test the idea of an mRNA (messenger RNA) vaccine in the newborn primate model. Although COVID-19 vaccines were the first mRNA-based ones to be approved, the technology has been in development for decades. For Alexander-Miller’s work, the results so far look promising, and the mRNA vaccine approach appears less sensitive to high levels of maternal antibodies interfering with the vaccine response, which makes it particularly valuable in newborns.
Universal appeal/approach
Another avenue of research, especially with influenza, is a universal vaccine that would cause the immune system to target a part of the virus that does not change or mutate from year to year. Currently, the immune system doesn’t make a strong response to that part, like it does to the part that changes every year.
“Adjuvants seem to really help to boost the response to that particular region, so I think there is hope for the future to perhaps not to have get a vaccine every year,” says Alexander-Miller. Decreasing the frequency or number of vaccines needed for immunity could increase the public’s willingness to get them. This would not only lead to fewer deaths from disease but also increase herd immunity, which protects people who can’t get vaccinated or don’t respond to the vaccine, including the very young and the very old.
Until a universal vaccine is developed and approved, though, Alexander-Miller and other members of the Center for Vaccines at the Extremes of Aging have plenty of questions to answer, theories to test and experiments to run.
“We might hit something that works on both ends of the spectrum or we might not,” says Alexander-Miller. “Or perhaps we need to think of them as individual groups, so there would be a vaccine for infants under 6 months of age that differs from a vaccine for those that are 6 months to 60 years of age, and yet another vaccine for the older population. It’s not one size fits all.”
